Overview
In the battle against COVID-19, the need for novel therapy has never been more urgent. While conventional treatments have shown promise, the quest for more potent solutions for severe and hospitalized cases continues.
Enter plasmapheresis – a versatile medical technique that has long been used to tackle various conditions. Scientists are now turning their attention to its potential to save lives threatened by the deadly grip of COVID-19.
Find out how plasmapheresis can build hope that may hold the key to curbing the threats and saving more lives.
Beyond Conventional Treatments: Plasmapheresis and Its Impact on Patient Survival
What Is Plasmapheresis?
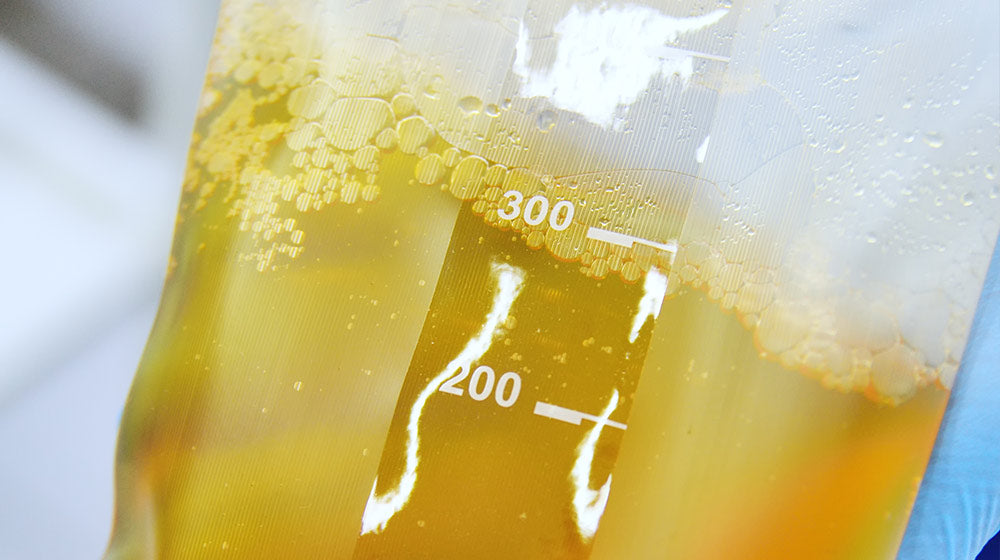
Plasmapheresis is a medical marvel that helps in treating various complex conditions. It works by selectively removing the liquid portion of your blood, called plasma, which contains various substances like antibodies and proteins.
The plasma is then replaced with a suitable substitute or fresh donated plasma before being returned to your body. This procedure is like cleansing your bloodstream thoroughly, targeting specific elements that may be causing health issues.
Why Do We Need Plasmapheresis?

Plasmapheresis is a crucial treatment option for many conditions, especially those where traditional medications might not be sufficient. Some common conditions that can benefit from plasmapheresis include:
- Autoimmune Disorders: When your immune system turns against your body, causing diseases like myasthenia gravis, lupus, or rheumatoid arthritis, plasmapheresis removes harmful antibodies to stop these autoimmune responses.
- Neurological Disorders: Conditions such as Guillain-Barre syndrome and chronic inflammatory demyelinating polyneuropathy (CIDP) can be managed with plasmapheresis to alleviate nerve damage and improve symptoms.
- Blood Disorders: Plasmapheresis helps control certain blood-related diseases like thrombotic thrombocytopenic purpura (TTP) and hemolytic uremic syndrome (HUS).
- Transplant Rejections: Plasmapheresis is used to filter out antibodies that might attack the new organ to prevent organ rejection after transplantation
- Toxin Removal: Plasmapheresis can help eliminate harmful substances from the bloodstream in poisoning or drug overdose cases.
How Does Plasmapheresis Work?
Understanding the plasmapheresis procedure is crucial for medical practitioners and patients alike. It involves aseptically drawing blood, selectively isolating plasma, and reintroducing filtered components to the patients.
- Connection: The procedure begins by inserting two intravenous catheters into the patient’s arm—one to draw blood from the body and the other to return.
- Separation: The patient’s blood enters a plasmapheresis machine, where it gets divided into its components. The plasma, along with the targeted elements, is separated and collected.
- Replacement: Depending on the treated condition, the collected plasma might be replaced with a suitable substitute or healthy donated plasma.
- Return: The filtered blood, with the replaced or discarded plasma, is then returned to the patient through the second intravenous catheter.
- Monitoring: Medical professionals closely monitor the patient’s vital signs throughout the procedure to ensure safety and efficiency.
Plasmapheresis Vs. Plasma Exchange
Plasmapheresis and plasma exchange are terms often used interchangeably but represent distinct steps within a comprehensive procedure.
- Plasmapheresis extracts plasma from the patient’s blood, isolating it to remove harmful components and sometimes replacing it with fresh donated plasma or a suitable substitute. This process allows the targeted removal of disease-causing substances and helps manage blood-related diseases.
- Plasma exchange replaces the patient’s plasma with healthy donated plasma without drawing blood. In this scenario, the patient solely undergoes the plasma replacement step. This approach mitigates transplant rejections, which remove harmful antibodies that attack the transplanted organ.
Is Plasmapheresis the Same as Dialysis?
Plasmapheresis and dialysis share the common principle of filtering harmful substances from the blood. Still, they are distinct procedures with different processes and indications.
- Plasmapheresis involves selectively removing the plasma from the blood, focusing on eliminating disease-causing elements like autoantibodies or toxins.
- Dialysis primarily targets the filtration of waste products and excess fluids from the blood, benefiting patients with impaired kidney function. It is used in chronic kidney disease or acute kidney injury to balance electrolytes and fluid levels.
Plasmapheresis for Severe Viral Infections
Premises
COVID-19, caused by SARS-CoV-2, has led to a high mortality rate worldwide. The severity of the disease is associated with an excessive release of inflammatory mediators like cytokines, causing respiratory distress and multi-organ failure.
In severe cases, cytokine storms and T-cell lymphopenia are the leading causes of death:
- Cytokine storms are severe immune reactions when the body releases excessive inflammatory molecules called cytokines. These storms can lead to hyperinflammation, tissue damage, and organ failure.
- T-cell lymphopenia is the significant reduction in the number of T-cells, a type of white blood cell that plays a crucial role in immune responses. T-cell lymphopenia weakens the body’s ability to combat infections and may contribute to severe immune-related conditions.
In this context, plasmapheresis was speculated to be capable of alleviating mortality caused by severe viral infections like COVID-19 by selectively removing pro-inflammatory factors and restoring immune responses.
Findings
A clinical trial was conducted to evaluate the impact of plasmapheresis on survival and cytokine release syndrome in severe COVID-19 patients.
Hospitalized patients aged 16 to 65 diagnosed with COVID-19 and cytokine storm syndrome were selected to test on plasmapheresis or standard therapy. Among them, 20 received plasmapheresis and were compared against 40 on standard therapy.
The design and details of the study are as follows:
| Exchange Plasma Volume | 1.5 times the estimated circulating plasma volume based on Kapplan’s formula. |
| Blood Flow Rate | 75-150 ml/min. |
| Replacement Solution | 3% albumin at a flow rate of 100-1500 mL/h. Two fresh frozen plasma units were transfused after each session. |
| Anticoagulation | Unfractionated heparin at 30-40 IU/Kg/h. |
| Session Frequency | Two sessions were systematically performed 48 hours apart. |
| Cytokine Determination | Blood samples were collected before and after each session for cytokine analysis. |
| Lung Damage Determination | CT imaging was used to calculate the volume of lung damage before treatment and 10 days after the last session. |
| Outcomes | Primary: all-cause mortality within 60 days
Secondary: mechanical ventilation-free (MV-free) days, decreased inflammatory markers, hospital length-of-stay |
The result was astonishing.
Plasmapheresis reduced 60-day mortality (50% vs. 20%), pro-inflammatory mediators, and the volume of the affected lungs while increasing lymphocyte count.
Also, it increased the patient survival rate with only a few minor occurrences of hypotension and subsequent infections—significant adverse effects were avoided.
Still, although plasmapheresis did not affect mechanical ventilation, a process where a ventilator is used to assist breathing, it was associated with longer hospital stays.

What Does the Finding on Plasmapheresis Mean?
The findings from this study highlight the critical significance of plasmapheresis in reducing the mortality rate among COVID-19 patients. The procedure is a valuable and practical therapeutic approach to managing severe viral infections, including COVID-19.
The study also provides compelling evidence for incorporating plasmapheresis as a vital component in the treatment regimen for COVID-19 patients, potentially saving lives and improving overall prognosis in this pandemic.
However, while research on plasmapheresis treatment demonstrated favorable outcomes, limitations, such as the single-center design and limited sample size, might have influenced the result. Also, the control-case match was incomplete due to a reduced candidate number, and the heterogeneity of the therapy posed challenges in data analysis.
Can Plasmapheresis Replace Conventional Treatments?
Several treatment options are currently used for COVID-19. These treatments control viral replication, reduce inflammation, and manage symptoms. They include:
- Antiviral drugs
- Corticosteroids
- Immunomodulators
Antiviral drugs, such as Remdesivir, have shown efficacy in reducing hospitalization time, while corticosteroids like Dexamethasone alleviate severe symptoms. Immunomodulators like Tocilizumab helps control cytokine storms, a cause of mortality in severe cases.
Still, they come with limitations.
Antivirals may not work for all patients, and corticosteroids could lead to a suppression of the immune system. Moreover, not all patients respond to immunomodulators, and their use requires careful consideration due to potential side effects.
Plasmapheresis has likely emerged as a promising adjunctive therapy, particularly in severe cases with cytokine storms. Removing pro-inflammatory factors complements existing treatments and can enhance their effectiveness.
However, plasmapheresis cannot entirely replace conventional treatments due to its selectivity in addressing specific aspects of the disease. Therefore, A comprehensive approach combining different treatment modalities should be a better option.
Plasmapheresis Safety and Considerations
Plasmapheresis is generally considered a safe procedure when performed by trained medical professionals. However, like any medical intervention, it may have potential side effects and risks that patients should consider carefully.
Whether it is used for conditions designated for plasmapheresis or viral infections like COVID-19, patients should weigh the benefits against the risks and make informed decisions in consultation with their healthcare providers.
Side Effects
- Low Blood Pressure: During the procedure, there is a risk of a drop in blood pressure, which may cause dizziness or fainting.
- Allergic Reactions: Some patients may experience allergic reactions to the replacement fluid or anticoagulants used during the procedure.
- Infections: Plasmapheresis involves inserting a catheter into the blood vessels, which can increase the risk of infection.
- Clotting: There is a risk of clot formation during the procedure, leading to complications like deep vein thrombosis.
Contraindications
- Unstable Cardiovascular Status: Patients with heart conditions or heart surgery should avoid plasmapheresis due to the risk of worsening cardiovascular status.
- Bleeding Disorders: Patients with bleeding disorders or low platelet counts should not undergo plasmapheresis to avoid the risk of excessive bleeding.
- Severe Anemia: Plasmapheresis can exacerbate severe anemia, so it should be avoided in patients with critically low red blood cell counts.
- Active Infections: Patients with active infections may have compromised immune systems, making them susceptible to complications during plasmapheresis.
- Severe Hypotension: Plasmapheresis may worsen hypotension in patients with low blood pressure.
Bottom Line
As the medical community delves deeper into the therapeutic potential of plasmapheresis, it stands as a beacon of hope in these challenging times. With lives hanging in the balance, pursuing innovative solutions like plasmapheresis keeps us firmly on the path to victory against the invisible foe that is COVID-19.
References
Fonseca-González G. et al. (2023). Impact Of Plasmapheresis On Severe COVID-19.
If you have questions about plasmapheresis or any health problems discussed here, contact us and learn more.
At Peak Human, our team of healthcare professionals helps you reach your ‘peak’ health with a custom whole-person approach. Using the most cutting-edge, science-backed biohacking and aesthetic tools available today, we help you achieve the highest physical/cognitive performance state, improving your overall quality of life.
Don’t hesitate to contact us for questions or to book an appointment. Get personalized support and insight from expert physicians.
UP NEXT: